Débora Gottardo Morello1, Isabela Reis Manzoli2, Alexsandro Klingelfus2, Diego Bezerra Soares2, Angélica Eloísa Casagrande2, Edineia Araújo de Alencar Brandão2, Adriana Kuttert Gazdzichi2, Diana Ferreira Puerari da Silva2, Karina Aparecida Santana2, Plínio Marinho de Carvalho Júnior2, Heloísa Ricardo Talau2, Eduardo Teixeira Silva2, Maria Gottardo Morello3
1 Evangelista Morello Health Unit, Morello/ES, Brazil
2 Uninassau University Center, Cacoal/RO, Brazil
3 Unesc University Center, Colatina/ES, Brazil
Received: 27 July 2024
Revised: 4 August 2024
Accepted: 4 August 2024
Published: 4 August 2024
Keywords:
Diagnostic approach, therapeutic management, multiple myeloma.
Corresponding author:
Débora Gottardo Morello
Doctor at the Evangelista Morello health unit, Morello/ES, Brazil
degottardo@gmail.com
doi: 10.5281/zenodo.13239313
ABSTRACT
| This research aimed to observe whether there is agreement between examiners in the interpretation of periapical radiographs to control endodontic treatment, seeking to establish a relationship between the quality of the filling and the occurrence of periapical lesions. To this end, 20 periapical radiographs were used, of which 10 radiographs corresponded to the immediate postoperative period and 10 control radiographs, of 10 completed endodontic treatments, carried out at the Faculty of Dentistry of Pernambuco. Three professors from the Endodontics Specialization course at this same educational institution were asked to evaluate the radiographs of the 10 endodontic treatments and to answer a questionnaire regarding the aforementioned cases. Radiographic analysis of root canal fillings was carried out under appropriate conditions for proper interpretation. Regarding inter-examiner agreement, it was found that, in relation to the periapical condition, examiners 1 and 2 presented a coincidence in 50% of cases, examiners 1 and 3, in 60%, and examiners 2 and 3, in 70%. %. Regarding agreement regarding the root canal filling limit, it was observed that examiners 1 and 2 agreed in 100% of cases and examiners 1 and 3, and 2 and 3, in 90% of cases. Providing an average inter-examiner agreement of 60% in the first assessment and 93.33% in the second assessment. Based on the results obtained, it is concluded that there was a high level of agreement between the examiners and that this may be related to the vast experience of the observers. |
INTRODUCTION / INTRODUÇÃO
Multiple myeloma is characterized as a malignant hematologic neoplasm, resulting from an unregulated proliferation that affects plasma cells in the bone marrow. Consequently, these cells excessively produce and secrete an anomalous monoclonal immunoglobulin, called M protein, causing suppression of humoral immunity and susceptibility to opportunistic infections, in addition to systemic symptoms such as bone destruction, hypercalcemia, renal failure and impaired hematopoiesis (1,2). Furthermore, the etiology is not yet well defined; studies point to multifactorial aspects involving heredity and genetic factors, as well as environmental components such as exposure to radiation and toxic substances such as benzene, immunosuppressive therapy, chronic inflammatory and autoimmune diseases, which appear to be related to the emergence of this pathology (2,3).
In this context, it is worth noting that multiple myeloma accounts for 1% of all malignant neoplasms and 10% when compared to hematologic neoplasms, establishing itself as the second most prevalent oncohematologic disease, second only to lymphomas3,4.Its annual incidence is around 4/100,000 inhabitants, there are more than 32 thousand new cases diagnosed in the United States per year and almost 13 thousand patients die, being more common in men than in women and twice as prevalent in individuals of African descent. The average age of patients at the time of diagnosis is approximately 65 years, with only 2% of cases occurring in people under 40 years of age (4,5).
The most common symptoms are: bone pain, fractures, hypercalcemia, kidney damage due to the accumulation of M proteins, anemia and increased blood viscosity. On the other hand, some patients may be asymptomatic, and the disease is discovered by chance through laboratory tests that reveal anemia, hyperproteinemia and impaired renal function. This neoplasm may present periods of remission and relapse, and may be asymptomatic or symptomatic depending on the functional and organic impairment of the patients (5,6). The differential diagnosis of multiple myeloma should be made with monoclonal gammopathy of undetermined significance, bone metastases of solid neoplasms and primary systemic amyloidosis.
METHODS
This study was prepared based on a retrospective review of the literature using the PubMed, Medline and SciELO databases. The descriptors used were “Abordagem Diagnóstico” (Diagnostic Approach), “Múltiplo Mieloma” (Multiple Myeloma), “Manejo Terapêutico” (Therapeutic Management) and their English equivalents “Diagnostic Approach”, “Multiple Myeloma”, “Therapeutic Management”. The Boolean descriptor used was “AND” for the database search. The exclusion criteria were: articles that do not correlate with the theme of the diagnostic and therapeutic approach to multiple myeloma, as well as articles published that do not cover the period studied from 2009 to 2024.
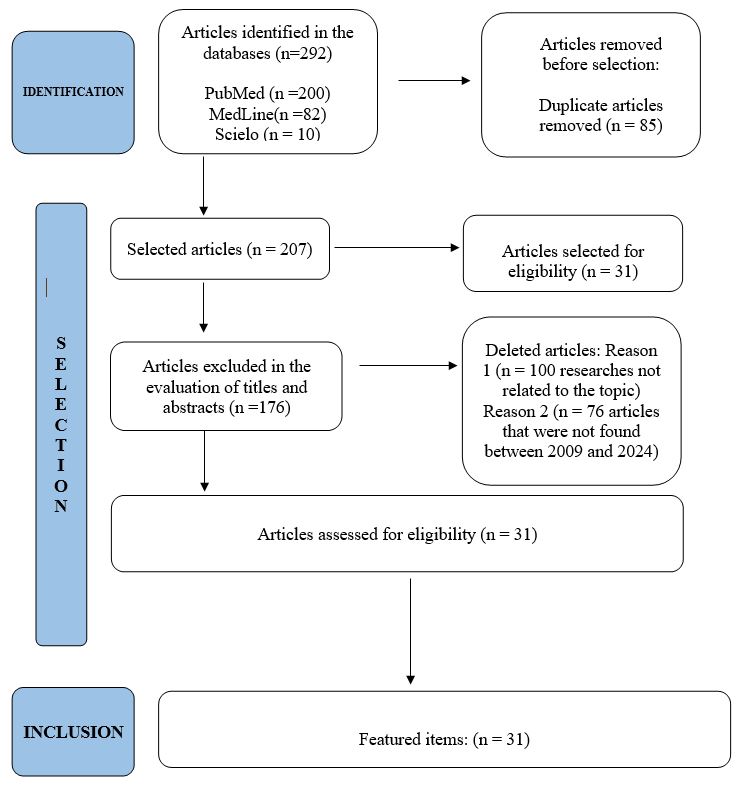
Figure 1. Prism method of research presented.
A total of 292 articles were found, adding up all the databases. After reading the titles of the articles, it was observed that some of them did not meet the inclusion criteria for this study. Thus, it was possible to remove 85 duplicate articles and 207 articles were selected for reading the abstract. Of these, 176 studies were removed based on abstract analysis and did not meet the objective of elucidating the diagnostic methods and therapeutic management of multiple myeloma as well as its preponderant factors, resulting in 31 full texts included in this literature review. The selection criteria were studies that had to meet the following criteria: studies published in English and Portuguese, systematic reviews, case reports, clinical studies and articles published between 2009 and 2024 (Figure 1).
RESULTS AND DISCUSSIONS
From this study, it was possible to observe that in the clinical context, the diagnosis of multiple myeloma can be established when at least two of the three criteria are met: bone lesions, presence of monoclonal immunoglobulin in serum or urine and excess plasma cells in the bone marrow generally above 10% detected through a bone marrow biopsy (7,8). In addition, other complementary tests, such as protein electrophoresis, immunofixation and renal function tests, can be used to confirm the diagnosis and assess the extent of the disease as well as its functional impairment (8,9).
Although well established, the diagnostic criteria were revised in 2015 by the International Myeloma Working Group (IMWG), which promoted a change in the clinical definitions aiming to elucidate the diagnosis and prevent target organ damage. In the update, the following are necessary for the diagnosis: evidence of target organ damage that can be attributed to the underlying plasma cell proliferative disorder, specifically present, as in hypercalcemia, with serum calcium >0.25 mmol/l (>1 mg/dl) greater than the upper limit of normal or >2.75 mmol/l (>11 mg/dl), in Renal failure taking into account creatinine clearance <40 ml per minute or serum creatinine >177 mmol/l (>2 mg/dl), in anemia with hemoglobin value >2 g/dL below the lower limit of normal, or hemoglobin value <10 g/dL and in bone deformities characterized by one or more osteolytic lesions on skeletal radiographs, computed tomography (CT) or positron emission tomography-CT (PET-CT). In addition, it is worth noting the presence of three specific biomarkers: percentage of clonal plasma cells in the bone marrow with a value >60%, involved/uninvolved serum free light chain (FLC) ratio >100, the involved free light chain level must be >100mg/L) and >1 focal lesion on MRI scans at least 5 mm in size. Furthermore, each of these biomarkers is associated with an 80% risk of progression to symptomatic target organ damage in two or more independent studies. The updated criteria represent a paradigm shift, as they allow early diagnosis and initiation of therapy before target organ damage (2,8).
In the context of imaging diagnosis, radiography is the most commonly used initial examination, with a sensitivity of 75% of cases, and the findings of plasmacytoma and myelomatosis generally show elliptical lesions of uniform size that form areas of destruction and osteopenia. Computed tomography can also be requested, capable of visualizing osteolytic lesions, diffuse osteopenia, fractures, bone sclerosis and the famous finding in the “Salt and Pepper Sign” image on CT of the skull referring to multifocal lytic lesions of various sizes in the cranial vault caused by trabecular bone resorption (10,11). Finally, magnetic resonance imaging, which is more accurate, allows the exclusion of focal lesions of the bone marrow, the evaluation of extramedullary diseases and spinal cord compression, the monitoring of disease progression and when detailed images of a specific symptomatic area are necessary (11,12).
Furthermore, in the clinical setting of multiple myeloma, patients should be tested for the presence of M proteins using a combination of tests that should include serum protein electrophoresis (SPEP), serum immunofixation (SIFE), and serum FLC assay. In this context, M protein measurement is considered when ≥1 mg/dL can be identified in serum and/or ≥200 mg/day in urine. Thus, the M protein level is monitored by SPEP and serum FLC assay to assess response to treatment during treatment and every 3-4 months when off therapy. Serum FLC assay is necessary in patients who do not have a measurable M protein, provided that the FLC ratio is abnormal and the FLC level involved is ≥100 mg/L. Urine protein electrophoresis is recommended at least once every 3–6 months to monitor the level of M protein in the urine and detect renal complications that may result in albuminuria (13,14).
Regarding the treatment of multiple myeloma, studies show that in symptomatic patients who present organic lesions, such as anemia, hypercalcemia, bone lesions, renal injury, hyperviscosity, amyloidosis and recurrent bacterial infections, treatment should be started early. In asymptomatic patients, no additional improvement was observed when starting chemotherapy at the time of diagnosis (14,15). Given the various existing therapeutic options, the initial impact of therapy with thalidomide, bortezomib and lenalidomide stands out, these immunomodulators and the numerous drugs used in cell therapy have significantly increased patient survival in the last 15 years, mainly because these drugs act with anti-angiogenic, immunomodulatory and tumor necrosis factor alpha inhibitory properties that cause cytotoxicity in tumor cells15,16. Generally, patients undergo 3-4 cycles of induction therapy and when eligible, the option is autologous transplantation, in which the patient’s own cells are used. Peripheral stem cells are indicated for patients resistant to chemotherapy and under 65 years of age, mainly because peripheral cells present a lower risk of contamination by neoplastic cells when compared to bone marrow cells (16,17).
To this end, it is necessary to perform pre-transplant therapy by administering an alkylating compound responsible for eliminating tumor cells. During the procedure, multiple chemotherapy agents may be used, and agents that produce myelosuppression should be avoided in order to collect peripheral cells. Some pre-transplant induction regimens lead to complete remission, i.e., absence of M protein and plasma cell counts of less than 5% in the bone marrow, a result of up to 10% of patients. The mortality rate of this treatment is around 1 to 2%, with a complete remission rate in 40% of cases (17,18).
In addition, allogeneic transplantation can also be used, being indicated to treat a small number of patients, especially because it is limited by the small number of compatible donors and is not recommended for elderly patients due to the high risk of mortality, as many do not have good lung, heart and/or kidney conditions. When this technique is indicated, the ideal donor should be the patient’s sibling, since in this group they have a survival rate of up to 15 years. The mortality rate related to this treatment is 25% (18,19). In patients who are not candidates for transplantation, chemotherapy alone tends to be an option. The most commonly used chemotherapy agent is melphalan combined with prednisone. This combination presents a response in up to 60% of cases, generally as palliative treatment. This procedure is performed for symptomatic patients over 70 years of age or younger patients for whom transplantation is not viable. Due to disease progression, pain relief and disease stabilization indicate therapeutic benefit (19,20).
In cases of refractory or relapsed multiple myeloma, therapy aims to control the progression of the disease, using alkylating agents obtained by combining immunomodulators, taking into account resistance to lenalidomide or not. It is worth noting that the choice of immunomodulators permeates many factors, including the response to previous therapy, aggressiveness of relapse, performance status and intrinsic aspects inherent to the patients (20,21). Furthermore, it is important to use, as an adjuvant to the main therapy, support measures based on the use of bisphosphonates that inhibit osteoclate-mediated bone resorption, reducing bone pain, decreasing hypercalcemia and the incidence of fractures, in addition to having a direct antitumor effect. Furthermore, erythropoietin administration can be performed to treat anemia, as well as to control renal failure (22,23). The Vertebroplasty and kyphoplasty are indicated for the treatment of vertebral bone deformities, which can cause fractures and spinal cord compression, which are extremely painful. Vaccination against pneumococci and influenza may also be indicated as supportive therapy, especially in patients undergoing treatment with myelosuppressants. Plasmapheresis is indicated in cases of symptomatic hyperviscosity, in addition to psychological support for the patient and their family (24,25).
In addition, supportive care for patients is recommended with zoledronic acid or pamidronate in all patients. A low-intensity regimen every 3–4 months may offer similar protection with fewer side effects compared to monthly administration. Additionally, denosumab, a high-affinity monoclonal antibody targeting RANKL, is an alternative, especially in patients with significant renal dysfunction. Upon discontinuation, a bisphosphonate dose should be considered to prevent osteoclast rebound activity (26-28).
Recent guidelines for the prevention and management of infections in myeloma demonstrate that patients with multiple myeloma do not respond adequately to COVID-19 vaccines and require boosters as recommended (28,29). Prophylactic levofloxacin in the first 2–3 months of initial therapy should be considered to reduce the risk of serious infection. Prophylaxis with trimethoprim-sulfamethoxazole or an alternative agent against Pneumocystis jirovecii pneumonia should also be considered long-term in all patients receiving prolonged therapy with steroids or anti-CD38 monoclonal antibodies (28,30). Acyclovir or valacyclovir should be administered routinely as prophylaxis against herpes zoster in patients receiving proteasome inhibitors, anti-CD38 monoclonal antibodies, or elotuzumab. Intravenous immunoglobulin should be considered for hypogammaglobulinemic patients receiving daratumumab who develop frequent respiratory tract infections (28,31).
CONCLUSION
Therefore, it can be inferred that multiple myeloma is considered the second most prevalent oncohematological disease in the world and should be diagnosed and treated as quickly as possible. This approach determines the survival rate of patients, which can vary from a few months to several years depending on the progression and onset of the disease. The initial treatment of choice is through the immunomodulators thalidomide, bortezomib and lenalidomide, as well as the numerous drugs used in cell therapy. In eligible patients, the most effective therapy is autologous transplantation, which is indicated for patients under 65 years of age and resistant to chemotherapy. This therapeutic modality has low mortality and, therefore, should be preferred.
The Allogeneic transplantation has some limitations and, therefore, is not routinely used. Chemotherapy alone is performed only in patients who are not candidates for transplantation and patients over 70 years of age as palliative therapy. In patients with relapse, treatment aims to control the progression of the disease by combining immunomodulators resistant or not to the drug lenalidomide, in addition to the extrinsic and intrinsic aspects inherent to the patients. Furthermore, it is worth highlighting the importance of supportive care aimed at survival and a better quality of life for patients with multiple myeloma.
REFERENCES
- Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014; 15: e538-e548.
- Landgren O, Weiss BM. Patterns of monoclonal gammopathy of undetermined significance and multiple myeloma in various racial/ethnic groups: support for genetic factors in pathogenesis. Leukemia. 2009; 23: 1691-1697.
- Rajkumar SV, Kumar S. Multiple myeloma current treatment algorithms. Blood Cancer J. 2020; 10: 94.
- Ito T, Ando H, Suzuki T, et al. Identification of a primary target of thalidomide teratogenicity. Science. 2010;327(5971):1345-1350. doi:10.1126/science.1177319
- Krönke J, Udeshi ND, Narla A, et al. Lenalidomide causes selective degradation of IKZF1 and IKZF3 in multiple myeloma cells. Science. 2014;343(6168):301-305. doi:10.1126/science.1244851
- Lu G, Middleton RE, Sun H, et al. The myeloma drug lenalidomide promotes the cereblon-dependent destruction of Ikaros proteins. Science. 2014;343(6168):305-309. doi:10.1126/science.1244917
- Rajkumar SV, Jacobus S, Callander NS, et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomized controlled trial. Lancet Oncol. 2010; 11:29-37.
- Krishnan A, Pasquini MC, Logan B, et al. Autologous hemopoietic stem cell transplantation followed by allogeneic or autologous hemopoietic stem cell transplantation in patients with multiple myeloma (BMT CTN 0102): a phase 3 biologic designation trial. Lancet Oncol. 2011; 12: 1195-1203.
- Kumar SK, Lee JH, Lahuerta JJ, et al. Risk of progression and survival in relapsed multiple myeloma after IMiDs and bortezomib therapy: a multicenter study from the international multiple myeloma working group. Leukemia. 2012; 26: 149-157.
- Hillengass J, Usmani S, Rajkumar SV, et al. International myeloma working group consensus recommendations on imaging in monoclonal plasma cell disorders [published correction appears in Lancet Oncol. 2019 Jul;20(7):e346. doi: 10.1016/S1470-2045(19)30423-1]. Lancet Oncol. 2019;20(6):e302-e312. doi:10.1016/S1470-2045(19)30309-2
- Hillengass J, Moulopoulos LA, Delorme S, et al. Whole-body computed tomography versus conventional skeletal survey in patients with multiple myeloma: a study of the International Myeloma Working Group. Blood Cancer J. 2017;7(8):e599. Published 2017 Aug 25. doi:10.1038/bcj.2017.78
- Dispenzieri A, Kyle R, Merlini G, et al. International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders. Leukemia. 2009;23(2):215-224. doi:10.1038/leu.2008.307
- Kumar SK, Dispenzieri A, Lacy MQ, et al. Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia. 2014;28(5):1122-1128. doi:10.1038/leu.2013.313
- Himelstein AL, Foster JC, Khatcheressian JL, et al. Effect of longer- vs standard-dose zoledronic acid on skeletal events in patients with bone metastases: a randomized clinical trial. JAMA. 2017; 317:48-58.
- Nea R. An international, randomized, double-blind study comparing denosumab with zoledronic acid (ZA) for the treatment of bone disease in patients with newly diagnosed multiple myeloma. 16th International Myeloma Workshop (IMW); March 1-4, 2017; New Delhi, India, Abstracts 546 2017, e28.
- Terpos E, Rajkumar SV, Leung N. Neutralizing antibody testing in patients with multiple myeloma after COVID-19 vaccination. JAMA Oncol. 2022; 8: 201-202.
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021; 71: 7-33.
- Silva ROP, Brandão KMA, Pinto PVM, et al. Multiple myeloma: clinical and laboratory characteristics at diagnosis and prognostic study. Rev Bras Hematol Hemoter 2009; 31 (02): 63 – 68.
- Katsekis KS, Kelham AS. Orthopedic treatment of multiple myeloma lesions. JBJS J Orthop Assistência Médica 2018; 6 (04): e40.
- Guedes A, Moreira FD, Mattos ESR, Freire MDM, Guedes AAL, Freire ANM. Orthopedic approach to bone metastases from carcinoma and multiple myeloma. Rev SBC 2022; 23 (62): 83 – 90.
- Guedes A. Multiple myeloma. In: Oliveira LG. Treatise on osteometabolic diseases. Goiânia: Kelps; 2020: 795 – 818.
- Sucro LV, Silva JCML, Gehlen GW, Eldin JFS, Amaral GA, Santana MAP. Multiple myeloma: diagnosis and treatment. Rev Med Minas Gerais. 2009; 19 (01): 58 – 62.
- Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk stratification, and management. Sou J Hematol 2020; 95 (05): 548 – 567.
- Guedes A, Barreto BG, Andrade RM. Metastasis of carcinoma, multiple myeloma and pathological fractures of the appendicular skeleton. In: Daltro GC. Health of the elderly: Locomotor system, physical condition and aging. Salvador: Author’s Ed.; 2016: 227 – 231.
- Grammatico S, Scalzulli E, Petrucci MT. Solitary plasmacytoma. Mediterr J Hematol Infect Dis. 2017; 9 (01): e2017052.
- Thumallapally N, Meshref A, Mousa M, Terjanian T. Solitary plasmacytoma: population-based analysis of survival trends and effect of various treatment modalities in the USA. BMC Cancer. 2017; 17 (01): 13.
- Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised International Staging System for Multiple Myeloma: A Report of the International Myeloma Working Group. J Clin Oncol. 2015; 33 (26): 2863 – 2869
- Rajkumar SV. Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am J Hematol. 2022;97(8):1086-1107. doi:10.1002/ajh.26590
- von Sucro L, da Silva JCML, Gehlen GW, et al. Multiple myeloma: diagnosis and treatment. Rev Med Minas Gerais. 2009;19(1):58-62.
- Himelstein AL, Foster JC, Khatcheressian JL, et al. Effect of longer-interval vs standard dosing of Zoledronic acid on skeletal events in patients with bone metastases: a randomized clinical trial. JAMA. 2017; 317: 48-58
31.Raje NS, Anaissie E, Kumar SK, et al. Consensus guidelines and recommendations for infection prevention in multiple myeloma: a report from the international myeloma working group. Lancet Haematol. 2022; 9: e143-e161.6/S0099-2399(83)80092-2



